Improving Claims Management Efficiency and Accuracy with the Policy Claims Analysis Dashboard
Introduction
In the rapidly evolving healthcare industry, managing policy claims efficiently is paramount for ensuring customer satisfaction and operational effectiveness. Abbott Pharmaceuticals recognized the need to enhance their claims management process and implemented the “Policy Claims Analysis Dashboard.” This dashboard provides comprehensive insights into various aspects of claims data, enabling better decision-making and process improvements.
Objectives
The primary objectives of the Policy Claims Analysis Dashboard were:
- To provide a clear and comprehensive overview of claims data.
- To identify trends and patterns in claims submissions and settlements.
- To enhance the efficiency and accuracy of the claims management process.
- To support strategic decision-making with data-driven insights.
Dashboard Overview
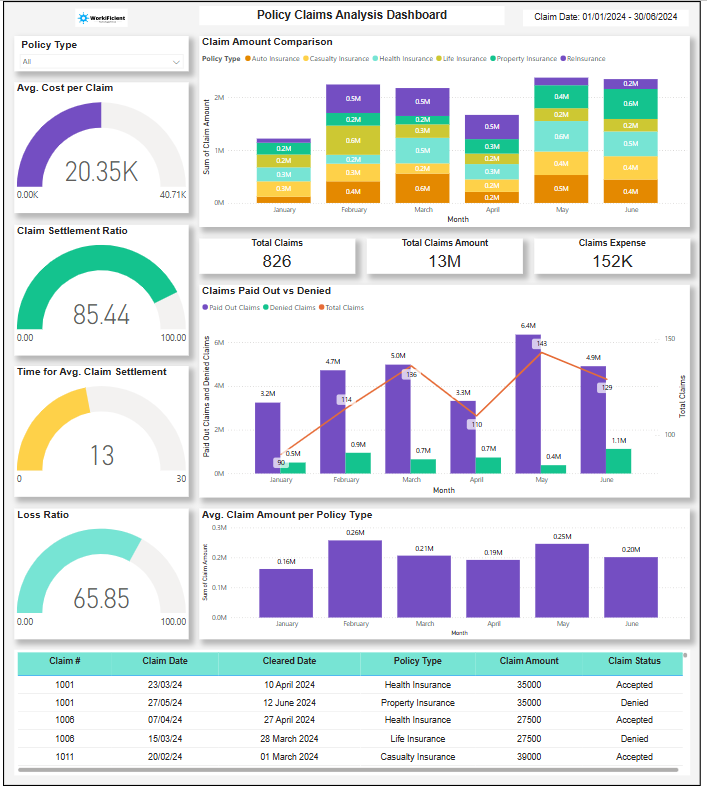
Selector: Policy Type
The dashboard includes a selector for policy types, allowing users to filter the data and analyze claims based on specific policy categories. This feature helps in identifying trends and issues related to different types of policies.
KPIs
The dashboard tracks several key performance indicators (KPIs) critical to assessing the effectiveness of the claims management process:
- Total Claims: The total number of claims submitted.
- Total Claims Amount: The cumulative value of all claims submitted.
- Claim Expense: The total expenditure on claim settlements.
- Cost Per Claim: The average cost incurred per claim.
- Claim Settlement Ratio: The ratio of claims settled to claims submitted.
- Time for Avg. Claim Settlement: The average time taken to settle a claim.
- Loss Ratio: The ratio of claims paid out to premiums earned.
Visualizations
- Claim Amount Comparison: This visualization compares the total claim amounts across different policy types, helping to identify which policies have the highest claim values.
- Claims Paid Out vs Denied: A comparative analysis of claims that were paid out versus those that were denied, providing insights into the approval and denial patterns.
- Claim Amount Per Policy Type: This visualization shows the average claim amount for each policy type, highlighting the cost associated with different policies.
- Claim Details: A detailed view of individual claims, including their status, amount, and processing time, offering granular insights into the claims data.
Impact and Improvements
Enhanced Decision-Making
The dashboard’s comprehensive visualizations and KPIs enabled the management team to make informed decisions. By identifying patterns and trends in claims data, the team could implement targeted strategies to address issues such as high denial rates and prolonged settlement times.
Improved Efficiency
The visualization of average claim settlement times and the claim settlement ratio provided insights into process bottlenecks. This information led to the optimization of the claims processing workflow, reducing the average time for claim settlement and increasing overall efficiency.
Better Financial Management
Tracking the total claims amount, claim expenses, and loss ratio allowed the finance team to manage resources more effectively. By understanding the financial impact of claims on different policy types, the team could allocate budgets more strategically and control claim-related expenses.
Increased Customer Satisfaction
With the dashboard highlighting the claims paid out versus denied, the team could identify and address reasons for claim denials. This proactive approach helped in reducing the denial rate, improving the claim settlement ratio, and ultimately enhancing customer satisfaction.
Strategic Insights
The analysis of average claim costs per policy type and claim amount comparisons provided strategic insights into policy performance. This information was crucial for product development and pricing strategies, ensuring that the company offered competitive and financially viable insurance products.
Conclusion
The implementation of the Policy Claims Analysis Dashboard at Abbott Pharmaceuticals significantly improved the claims management process. The dashboard’s ability to provide detailed insights and track essential KPIs enabled the company to enhance operational efficiency, financial management, and customer satisfaction. By leveraging data-driven insights, Abbott Pharmaceuticals achieved a more streamlined and effective claims process, demonstrating the value of advanced analytics in the healthcare industry.
Recommendations for Future Enhancements
- Integration with Real-Time Data: Implement real-time data integration to provide up-to-date insights and enable prompt decision-making.
- Advanced Analytics: Incorporate predictive analytics to forecast future claims trends and identify potential issues before they arise.
- User Training: Conduct training sessions for users to fully utilize the dashboard’s features and extract maximum value from the insights provided.
This case study exemplifies how leveraging a well-designed dashboard can lead to substantial improvements in managing policy claims, driving both operational excellence and customer satisfaction in the healthcare industry.
